Tumours of the salivary glands
Tumours of the salivary glands are rare tumours among children and adolescents. They can be benign or malignant. With this text, you will receive information on the disease, symptoms, causes, diagnosis, treatment and prognosis.
Author: Prof. Dr. med. Dominik T. Schneider, Dr. med. Ines Brecht, Editor: Maria Yiallouros, English Translation: Dr. med. Gesche Riabowol (nee Tallen), Last modification: 2024/05/30 https://kinderkrebsinfo.de/doi/e174315
Table of contents
Both benign and malignant tumours can develop in the salivary glands. This, however, happens rarely both in children as well as in adults. In Germany, approximately ten children or teenagers are diagnosed with such a tumour per year.
Hence, there are no therapy studies providing the optimal treatment strategy that has been proven for many patients, as there are for other tumours in childhood and adolescence. However, the experts of the Registry for Rare Diseases in Paediatrics (German abbreviation: STEP, for “Seltene Tumorerkrankung in der Pädiatrie”) have summarized their experiences as well as the experiences of international research groups on the following pages.
Since every child is different, it is important to individually adjust the treat-ment to every single patient. Therefore, “STEP” offers free advice via a tumourboard attended by multidisciplinary experts. Feel free to have your attending physician contact the experts at “STEP” at step@klinikumdo.de. Also, by registering your child with the „STEP“ registry, you get the option to help expanding the experience with these rare tumours, thereby helping other children who are diagnosed with such a disease in the future.
Introduction to the salivary glands
The salivary glands are located in the area of the lower jaw. They are responsible for producing saliva. Saliva moistures our intaken food while chewing, thereby making it smooth. Saliva contains certain enzymes (so-called amylases) which predigest – to a limited degree – carbohydrate-rich food. Saliva also contains an antibacterial substance that promotes the inactivation of pathogens.
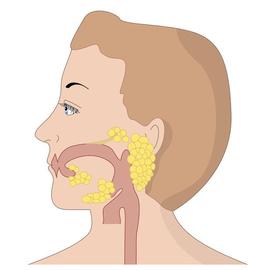
(© Martha Kosthorst - Fotolia.com)
There are three pairs of large salivary glands:
The largest are located in front of the parotid glands (Glandulae parotideae). The facial nerve (Nervus facialis), which innervates the facial muscles and controls facial expression, goes through them.
In addition, there are the two submandibular (Glandulae submandibularis) and the sublingual salivary glands (Glandulae sublingualis).
Disease: what is a tumour of the salivary glands?
Salivary gland tumours arise from salivary gland tissue. Most of the tumours develop in the parotid glands, however, the other salivary glands can also be affected.
There are a few different tumours in this area. Benign and malignant tumours are equally common.
The most common benign salivary gland tumour is pleomorphic adenoma. The most frequent malignant tumour in children and adolescents is the so-called mucoepidermoid carcinoma, followed by acinar cell carcinoma. These tumours behave less aggressively than other carcinomas mostly occurring in adults. This means that they grow more slowly and spread less frequently into the lymph nodes or other organs (metastasis).
Cause: how does a tumour of the salivary glands develop?
The exact cause of developing a salivary gland tumour is unknown. Most tumours occur sporadically. That means that there are no familial genetic risks. Different from adults, there are also no known risk factors for most children.
It is known, though, that the risk for these tumours is increased after radiotherapy of another cancer in this area. Occasionally, salivary gland tumours have been observed after chemotherapy for leukaemia treatment.
Symptoms: what are the signs of the disease?
Patient with a salivary gland tumour may not have any complaints for a while. First indication of the disease is often a visible and palpable, usually indolent, swelling. Some children may have impaired facial expression, such as a wry smile or slurred speech, which indicate damage of the facial nerve.
The following signs of the disease (symptoms) may occur, particularly with advanced stage:
- swelling
- decreased salivation, dry mouth
- pain, facial sensory deficits
- unilateral paralysis of facial muscles
Diagnosis: what kinds of tests are required?
Usually, the paediatrician will first take a thorough medical history (anamnesis) and perform a physical examination. There are no laboratory results that are specifically indicative of a salivary gland tumour. When palpation and/or symptoms are suspicious of a tumour, imaging diagnostics will help find out whether this is the case.
Ultrasound (sonography), magnetic resonance tomography (MRT, layered scanning of the body using magnetic fields and radio waves) and/or computed tomography (CT, detailed x-ray slices of the body) help to obtain information on the tumour’s location, its size, extent and growth pattern. When dealing with children and adolescents, not using techniques based on X-rays is the goal, therefore, ultrasound and magnetic resonance tomography are the standards.
Obtaining a tissue sample is not mandatory, since surgical tumour removal is scheduled at the beginning of treatment.
Therapy: how is treatment done?
Treatment of children and adolescents with a tumour of the salivary glands should take place in a children’s hospital with a paediatric oncology program, in cooperation with an ear, nose and neck (ENT) clinic. Only such a childhood cancer centre provides highly experienced and qualified staff (doctors, nurses and many more), since they are specialised and focused on the diagnostics and treatment of children and teenagers with cancer according to the most advanced treatment concepts.
Therapy mainly consists of surgery aiming at tumour removal, sometimes followed by radiotherapy. Chemotherapy is applied very rarely.
Surgery
The major therapeutic step is gross total tumour removal. Since remaining tumour tissue is frequently followed by recurrent disease (relapse), tumours are being removed with a safety margin. That means that not only the tumour itself is being resected, but also an appropriate amount of adjacent healthy tissue as well. Taking out the entire salivary gland or its affected lobe in total is considered safest.
However, if the tumour is located in the parotid gland, the facial nerve needs to be spared so that surgery does not cause subsequent facial paralysis. This procedure may be complicated, particularly when dealing with larger tumours. Therefore, tumour resection should always be performed by an experienced ENT surgeon who also has experience with treatment of these tumours. For its protection, the facial nerve is permanently monitored during surgery (neuromonitoring).
In case of lymph node involvement, surgery needs to be extended to the affected lymph nodes and adjacent tissue. This procedure is known as neck dissection.
Additional treatment options
Benign tumours (adenomas) do not require additional treatment following surgery. For most malignant salivary gland tumours in childhood and adolescence, therapy is ceased after gross total resection, too. If complete removal is not feasible or in case of metastasis, additional therapy needs to be considered. In general, chemo- or radiotherapy are the options.
For localised tumours, radiotherapy is more efficient. However, the risk of radiotherapy-associated long-term sequelae require consideration. According to the currently available data, children and adolescents more frequently develop complications after radiotherapy than adults (for example impaired facial growth, secondary malignancies). Therefore, radiotherapy should be only applied for selected patients and after careful consideration, for example when the tumour could not be completely removed or in case of an aggressive tumour type.
Only in extremely rare scenarios, chemotherapy is required in children and adolescents. It is usually combined with radiotherapy. Since this is required in rare scenarios only, advice should be given by the inter-disciplinary tumour board for rare diseases.
Note: please confer in advance, feel free to contact the STEP Registry step@klinikumdo.de).
Prognosis: what are the chances of cure?
Children and adolescents with a tumour of the salivary glands usually have a very good prognosis. Most patients in this age group become completely healthy. The outcome is mostly impacted by the tumour type and the success of surgery. In general, gross total tumour resection is associated with a more favourable prognosis than partial removal.
It is good to know that benign tumours can also relapse after incomplete tumour resection. In this case, a benign tumour may occur again at the same location. However, malignant tumours, thus salivary gland carcinomas, in childhood and adolescence are usually rather minimally malignant (low-grade). This means that they metastasize very rarely and don’t grow aggressively locally.
The STEP Registry has analysed the data of all registered patients. About 10 % of children and adolescents developed a local relapse in the salivary gland or in the adjacent tissue, which was subsequently treated surgically again. Only extremely rare, very aggressive variants, such as the NUT midline carcinoma, take a malignant course. Hence, this tumour type requires the choice of a very intensive treatment from start.
Patients with parotid gland tumours can suffer injury of the facial nerve (Nervus facialis) and subsequent facial paralysis as a treatment complication after surgery. This happens in about 8 % of cases; the risk can be reduced by means of intraoperative neuromonitoring (IOM).
 Brief information on tumours of the salivary glands (169KB)
Brief information on tumours of the salivary glands (169KB)
Author: Maria Yiallouros
Status: 14/10/2023; glossary included 30/05/2024
References 
- Hippert F, Desing L, Diez S, Witowski A, Bernbeck B, Abele M, Seitz C, Erdmann F, Brecht I, Schneider DT: Rare Tumors in Children and Adolescents - the STEP Working Group's Evolution to a Prospective Registry. Klinische Padiatrie 2022, 234: 146 [PMID: 34798669]
- Achajew A, Brecht IB, Radespiel-Tröger M, Meyer M, Metzler M, Bremensdorfer C, Spix C, Erdmann F, Schneider DT, Abele M: Rare pediatric tumors in Germany - not as rare as expected: a study based on data from the Bavarian Cancer Registry and the German Childhood Cancer Registry. European journal of pediatrics 2022, 181: 2723 [PMID: 35478271]
- Surun A, Schneider DT, Ferrari A, Stachowicz-Stencel T, Rascon J, Synakiewicz A, Agaimy A, Martinova K, Kachanov D, Roganovic J, Bien E, Bisogno G, Brecht IB, Kolb F, Thariat J, Moya-Plana A, Orbach D: Salivary gland carcinoma in children and adolescents: The EXPeRT/PARTNER diagnosis and treatment recommendations. Pediatric blood & cancer 2021, 68 Suppl 4:e29058 [PMID: 34174160]
- Brecht IB, Bremensdorfer C, Schneider DT, Frühwald MC, Offenmüller S, Mertens R, Vorwerk P, Koscielniak E, Bielack SS, Benesch M, Hero B, Graf N, von Schweinitz D, Kaatsch P: Rare malignant pediatric tumors registered in the German Childhood Cancer Registry 2001-2010. Pediatric blood & cancer 2014, 61: 1202 [PMID: 24585499]
- Bisogno G, Ferrari A, Bien E, Brecht IB, Brennan B, Cecchetto G, Godzinski J, Orbach D, Reguerre Y, Stachowicz-Stencel T, Schneider DT: Rare Cancers in Children - The EXPeRT Initiative: A Report from the European Cooperative Study Group on Pediatric Rare Tumors. Klin Pädiatr 2012, 224: 416 [PMID: 23143769]
- Schneider DT, Brecht IB, Olson ThA, Ferrari A (Eds): Rare Tumors In Children and Adolescents. Series: Pediatric Oncology, Springer-Verlag 2012 [ISBN: 978-3-642-04196-9]
- Brecht IB, Graf N, Schweinitz D, Frühwald MC, Bielack SS, Schneider DT: Networking for children and adolescents with very rare tumors: foundation of the GPOH Pediatric Rare Tumor Group. Klinische Padiatrie 2009, 221: 181 [PMID: 19437371]